November is National Diabetes Month. This rampant chronic disease can be debilitating and even deadly if left uncontrolled or mismanaged. In fact, about half of those with diabetes do not even know they have it! This is a dangerous place to be, and highlights the need to pay attention to risk factors and check glucose and insulin with your doctor. With diabetes affecting nearly 11% of the American population, raising awareness of this disease is critical, specifically during the COVID pandemic. As we have discussed, it is known that those with pre-existing medical conditions are more vulnerable to becoming severely ill from COVID-19, and diabetes is no exception. The CDC states that roughly 4 out of 10 people with COVID also have diabetes. This statistic should wake us up and spur us into action. We must be taking steps to prevent and even reverse type 2 diabetes while also keeping it well-managed. With a virus like COVID-19, we cannot afford to be at increased risk, especially when it is within our power to reduce that risk.
How Diabetes Increases Risk and Severity of COVID
You might be wondering how a virus is even linked to diabetes in the first place. I mean, one affects our immune system and the other affects our blood sugar. They seem like completely separate systems working independently of the other…right? Well, no. These systems are very much interconnected. Let’s find out how.
Through Chronic Inflammation:
Chronic disease of any kind (arthritis, IBS, COPD, heart disease, dementia) all have inflammation at its core. Diabetes is no different. Chronic disease leads to chronic inflammation. Inflammation is not meant to be chronic, however. It’s meant to occur quickly when there is acute injury or sickness, and this activates our immune system to jump into action and fight the threat. When inflammation is chronically activated….our immune system is also chronically activated. This puts stress on our immune system, making it hyper-responsive. This might sound like a good thing, but our bodies cannot exist in a constant hyper-responsive state. There must be an ebb and flow where body systems are activated, the threat is removed, and then body systems calm down. In essence, our immune system cannot keep up with the demand (just like insulin cannot keep up with the demand from high blood sugar). When any body system cannot keep up, it slows down. When our immune system is overworked dealing with chronic inflammation, it is slow to respond to acute threats, such as a bleeding hand or the flu. Our immune system then becomes weakened, which affects how well we can fight off viruses, including COVID.
Through High Blood Sugar:
Our immune system is not only affected by chronic inflammation. It is also affected by high blood sugar. Low and chronic inflammation damages our pancreas. The pancreas is where insulin is made and a damaged pancreas leads to decreased insulin production. With less insulin to escort glucose into our body cells, glucose now hangs out in our blood stream causing high blood sugar. Sugar molecules in our bloodstream can weaken our immune cells, making it harder to control the spread of infection. The exact mechanism of how high blood sugar weakens our immune response is still being researched, but one thing is clear: those with diabetes are more susceptible to infections.
Through Poor Blood Circulation:
Chronic inflammation and high blood sugar are enough reasons to weaken our immune system, right? Well, we have one more: narrow blood vessels. High blood sugar can stiffen blood vessels by reducing how well our vessels can dilate (called vasodilation). Stiffened blood vessels restrict blood flow and lead to poor circulation. This leads to high blood pressure, lack of oxygen in blood cells, and even cell death in our extremities (causing necrosis and amputation). Our circulatory system carries oxygen and nutrients throughout the body. It also carries immune cells. When we have low blood flow from narrow vessels, our immune cells cannot travel quickly or in the right numbers to the site of infection. Essentially, constricted blood vessels cause our immune fighters to not only arrive late but also to show up understaffed.
I Have Diabetes. What Can I Do To Protect Against COVID?
As we have learned, those with diabetes are put at increased risk for getting COVID for a few reasons: having chronic inflammation, elevated glucose levels, and poor blood circulation. These factors all lead to a compromised immune system. There are steps you can take to lower your risk of getting COVID, which includes addressing inflammation and high blood sugar.
Follow CDC Guidelines:
The guidelines laid out by the CDC, which we have covered before in previous blogs, are recommended for all people but are doubly important for those with diabetes and other chronic conditions. A short summary of these well-known CDC guidelines are below:
- Wash hands frequently
- Avoid touching your face
- Wear a mask when in public areas and when meeting with people
- Maintain a 6-foot distance between people when in public places
- Disinfect high-touch surfaces in your home and workplace frequently
- Avoid sharing food, utensils, towels, etc.
- Cover your mouth and nose when sneezing or coughing
- Avoid contact with anyone having respiratory symptoms, including a cough
- Avoid unnecessary travel, public transport, and large gatherings
Manage Your Diabetes:
In addition to following the above guidelines, those with diabetes should also follow specific action steps to manage their condition.
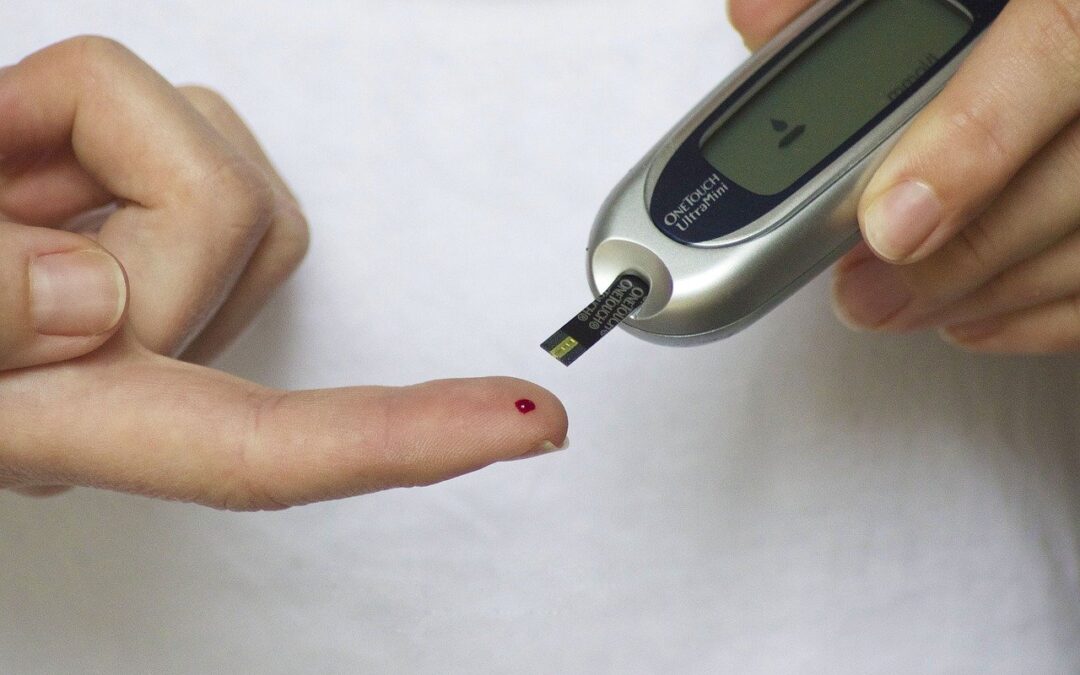
- Pay close attention to glucose levels through regular monitoring throughout the day, both before and after meals as well as upon waking up
- Stay hydrated throughout the day. Drinking plenty of water helps your kidneys flush out excess blood sugar through the urine
- Ensure you have enough insulin to carry you for a few weeks should you need to self-quarantine
- Always be prepared to quickly address sudden blood sugar drops, including while away from home or in the car
- If you live alone, alert a neighbor or nearby friend that you have diabetes and have them able to assist you if you become ill
- Keep a manageable schedule and avoid overworking and late nights
- Prioritize getting good sleep
- If you develop respiratory or flu-like symptoms, alert your doctor immediately. He or she can guide you in what to do and if you should be seen. Coughing up mucus can point to an infection and warrants immediate treatment
Get The Right Nutrition:
Choosing the right foods is the number one way to stabilize blood sugar and is a key component in managing diabetes. Additionally, the right nutrition focuses on anti-inflammatory foods, thus lowering chronic inflammation. Incorporate the following eating habits into your daily routine.
Pay attention to the Glycemic Index (GI) and Glycemic Load (GL) of the carbohydrates you eat.
- Carbs that have a low GI or GL slowly release glucose into your body, resulting in a healthy, steady rise and gentle fall. High GI or GL carbs, on the other hand, release glucose quickly, giving you a quick spike and impairing glucose control.
- Eat foods on the low end of these measurements. Food with a low Glycemic Index is anything under 55, while a low Glycemic Load is any food under 10.
- Glycemic Load is a more accurate measurement to follow. Many foods have a high Glycemic Index but a low Glycemic Load. When there is disparity like this, opt for low Glycemic Load.
- Pay attention to serving sizes! Eating large servings will quickly raise a low food measurement to a high food measurement.
- See this chart for a list of foods and their associated Glycemic Index and Glycemic Loads
Prioritize green leafy vegetables! These are packed with nutrients, many of which are not found in other foods in the right amounts. Further, most people are deficient in several of these nutrients, so it’s impossible to eat too many greens!
Eat healthy fats, primarily from plant foods. Healthy fats are omega 3 fatty acids and monounsaturated fatty acids. These fats are found in fish, nuts, chia seeds, flaxseeds, avocados, olives, quinoa, and eggs. Coconut oil is also very healthy, despite its saturated fat content.
Eat lean protein. This includes fish, lean meats, eggs, and beans
Avoid eating fried foods, such as French fries, fried chicken, fried seafood, mozzarella sticks, etc. Fried foods are made using harmful seed oils that increase inflammation
Avoid high-sugar foods and anything with added sugars. Whole fruit is an exception, in moderation (2 servings per day). Be aware that some fruits have a high Glycemic Load.
Form an Exercise Routine:
Workout facilities such as gyms, sports centers, public pools, or YMCA’s may be closed or have limits on how many people can enter. This needn’t discourage you from exercising though. There are several ways to exercise without going to a gym. Those with diabetes should especially increase their physical activity, as it is an important part of diabetes management. Any physical activity that increases your breathing and heart rate will draw more glucose into your muscles (and out of your bloodstream) while also increasing insulin sensitivity. Here are several ways to get moderate-intensity exercise into your day:
- If you have a treadmill or elliptical machine at home, aim for one hour of brisk walking. This hour can be divided into three 20-minute sessions if needed. Increasing the slope on the treadmill will provide additional benefits. Brisk walking around your neighborhood or along a trail provides these same benefits
- If you have a stationary bike, aim for 30 minutes (or two 15-minute sessions) while slowly increasing the pedal resistance. Lower the resistance during the last 2 minutes as you cool down. Biking along a trail or street provides these same benefits
- Bodyweight exercises are done without any equipment. These include push-ups, crunches, sit-ups, squats, lunges, and planks
- Hand weights and bands elevate the intensity and resistance of bodyweight exercises. Lifting hand weights, using resistance bands for your legs, or securing a handled band in a doorframe are great ways to vary your exercise routine
- Stretching exercises are great for joint mobility and lower-back muscles. Common stretches work just fine, as well as following a yoga or Pilates routine
- If you have stairs in your home and are more accustomed to exercise, challenge yourself to do 5 trips up and down the stairs
The link between diabetes and the COVID-19 virus is undeniable, with about 40% of COVID cases also having diabetes. The very nature of diabetes, its causes and symptoms, cause a downward cascade of events that ends with a weakened immune system and a delayed immune response. This allows any pathogen (viral, bacterial, or fungal) to more easily overcome our defenses causing active infection and symptoms. Fortunately, there are steps we can take to help prevent the COVID virus–by following CDC guidelines, managing diabetes, and eating nutrient-rich whole foods. The link between diabetes and COVID does not mean we give up. Rather, it motivates us to develop new habits, develop healthier lifestyles, and stay one step ahead of this pandemic.